Recently, the "Science Report" under the "Nature" Publishing House published a surprising study. Eight patients with spinal cord injuries who had been with the brain for many years, controlled their machines through the brain, and their muscle function and perception of the lower extremities were partially restore.

Brain-machine interfaces
This training is accomplished through the use of brain-machine interfaces (also called brain ports) in conjunction with virtual reality (VR) and machine exoskeletons. The whole process is probably like this. After wearing these three devices, the patient imagines the walking process through the virtual reality scene. After the brain-machine interface captures the nerve signals, it extracts the walking signals and instructs the machine's exoskeleton to take the lower limbs to do the corresponding actions.
This exciting study was led by neuroscientist Miguel Nicolelis, a renowned neuroscientist at Duke University in the United States. The study is part of the "Walk Again Project" in Sao Paulo, Brazil. This program is designed to allow those with spinal cord injuries and strokes. The patient who causes the paralysis, stands up again and achieves an independent life.
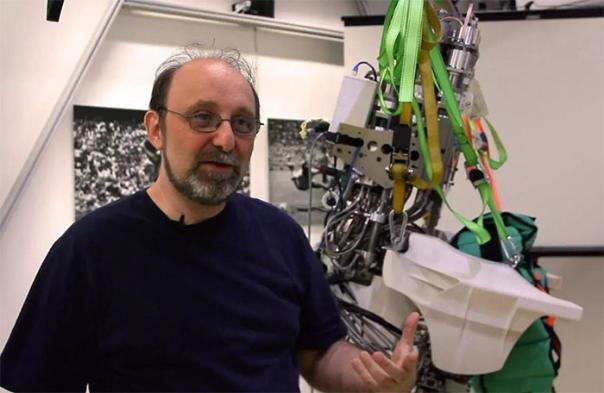
Professor Miguel Nicolelis and his equipment
When we started this project, we did not anticipate such amazing clinical results. Our results show that patients with paralysis use brain-computer interfaces to cooperate with VR and exoskeletons. After a period of training, they can improve their lower limb activities and perception, and even improve the function of some organs caused by paralysis (for example, Incontinence, etc.) Obstacles. Until now, no one has been able to reactivate people who have spent many years completely. Nicolelis, director of the Duke Neuroengineering Center in Brazil, said.
In this study, some patients began to undergo some changes after receiving 7 months of training. One year later, four patients had significant changes in the perception and muscle control of the lower extremities, so that doctors changed the diagnosis completely from one year ago to a partial one.

Patients with brain-computer interface and VR are learning to use training equipment
Most patients found their bladder control and intestinal function improved, and their dependence on laxatives and catheters was significantly reduced. Nicolelis said that these improvements can reduce the risk of death due to infection in patients with paralysis.
In recent years, researchers have begun to use brain-computer interfaces to establish connections between the patient's brain and computers and prostheses. In the past 20 years, Nicolelis has been working to establish and tune brain-computer interfaces. He has recorded hundreds of brain nerve signals. From signals that appear to be "disorganized," he extracted signals that control actions and used them. These signals successfully reproduce the corresponding actions on the exoskeleton.
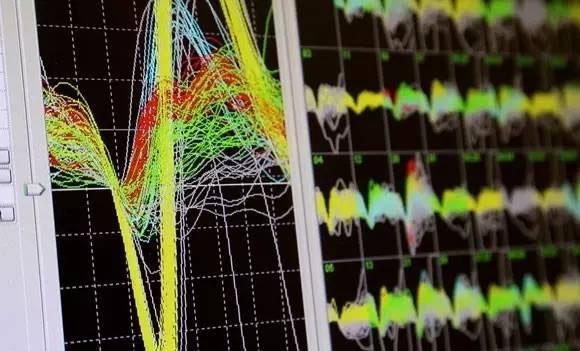
Analyze and process brain signals
Nicolelis and his colleagues firmly believe that through weekly training, spinal nerve signal pathways can be restored in patients who are paralysed by traumatic injuries such as car accidents and falls. This was also confirmed in this study. Among the recruited volunteers, five patients had been hospitalized for more than 5 years, and 2 patients had been hospitalized for more than 10 years. Almost all of them have been better restored.
In particular, the 32-year-old female patient who had been in 13 years, the changes that happened to her can be described as "dramatic." Before training, even if she was given support tools, she could not stand up; after receiving complete training, with support tools and the help of a doctor, she could walk. By 13 months, with the support of the seat belt, she can move her legs independently.

Training...
Nicolelis said that an earlier study found that most of the spinal cord nerves of the paralyzed patients are intact. Because of the signal interruption with the brain, those nerves lie there quietly and can be reactivated through brain-computer interfaces and exoskeletons. These sleepy nerves. Even if only a small part of the nerve remains intact, this training can also restore some of the body functions of the patient.
Up to now, almost all the volunteers who participated in the research of Nicolelis are still training. They have been trained for more than 2 years. Nicolelis and his colleagues are planning to publish follow-up study data for these patients. They also intend to conduct clinical studies on patients with very short periods of time. They want to know if the rapid progress of this treatment will make patients recover better and faster.
Of course, taking into account the cost and convenience of receiving treatment in hospitals, the Nicolelis team is also considering the development of a device that can be used at home.